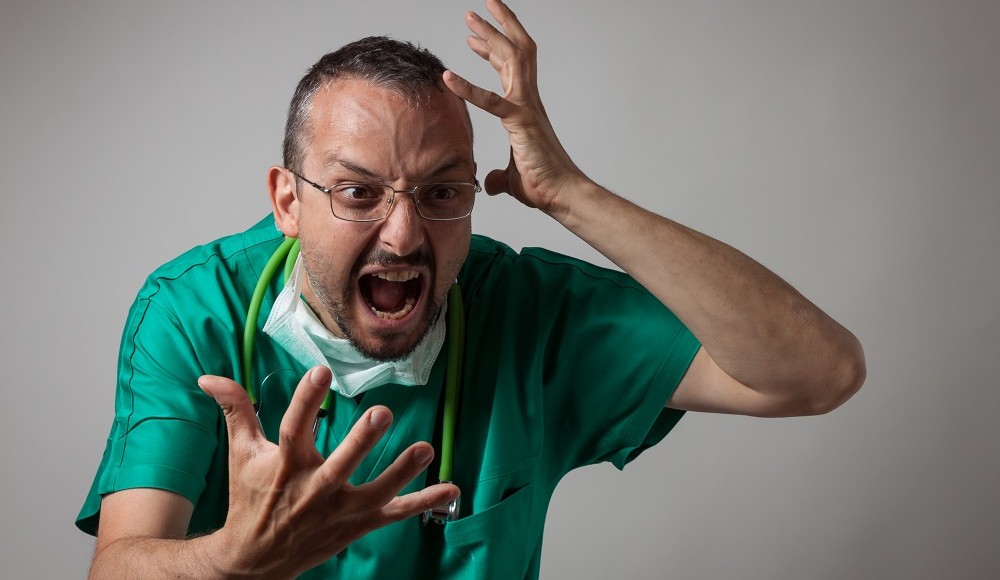
If cancer ran in your family, you would not wait until you contracted the disease before taking action; you would take preventative measures and possibly avoid cancer completely. Disruptive behavior in health care organizations is a cancer that can spread across departments harming staff members, patients, physicians and administrators along the way.
The Joint Commission released their Sentinel Event Alert (issue 40) “Behaviors that undermine a culture of safety” on July 9. It states that “intimidating and disruptive behaviors can foster medical errors, contribute to poor patient satisfaction and to preventable adverse outcomes, increase the cost of care, and cause qualified clinicians, administrators, and managers to seek new positions in more professional environments. Safety and quality of patient care is dependent on teamwork, communication, and a collaborative work environment.” As a result, effective January 1, 2009, new Leadership Standards will require health care organizations to address disruptive and inappropriate behavior in two ways: by creating a code of conduct that defines acceptable, disruptive and inappropriate behaviors, and by creating and implementing a process for managing disruptive and inappropriate behaviors.
The Alert suggests actions including the ones listed below. (Read the entire list of suggested actions at http://www.jointcommission.org/)
- Educate team members on appropriate professional behavior defined by the organization’s code of conduct and hold them accountable for modeling desirable behavior
- Develop and implement policies, procedures, and an organizational process to address intimidating and disruptive behaviors, including a reporting/surveillance system (possibly anonymous) for detecting unprofessional behavior
- Support surveillance with tiered, non-confrontational intervention strategies
Most of the suggestions are directed toward managing disruptive behaviors, rather than preventing them. Their prevention suggestions are limited to business etiquette and people skills training, none of which can be applied when self-awareness and self-management skills are absent or underdeveloped. While disruptive behavior management is valuable, it does not relieve frustration and make struggling professionals feel heard. Reducing the likelihood of or eliminating disruptive behaviors altogether is the more appropriate goal. After all, an ounce of prevention is half the cure.
What measures / programs could a health care organization offer?
Coaching for Work-Life Balance
In my work as a physician coach, I have seen many instances in which physicians were in crisis because they were out of balance in their lives. More and more health care professionals experience what I call “life balance fatigue,” where they are often
- more cynical, critical and sarcastic at the workplace
- irritable and less patient with colleagues, staff members and patients
- feeling that they face insurmountable hurdles at work
- having a hard time laughing at small glitches in daily life
- self-medicating using food, drugs or alcohol to feel better or to become numb.
While working with individual physicians, dissatisfaction and pressures in their personal and professional lives are often the underlying sources of inappropriate behaviors. I believe no health care professional gets up in the morning intending to physically threaten staff members or refuse to perform assigned tasks. The key is for physicians to develop skills that prevent disruptive behavior in the first place.
Supported Goal Setting
People who recognize that they are making constant progress and accomplishing goals are less frustrated than high-achievers who feel they are treading water. I have found that few physicians actually set goals. Yet being “self-actualizing” – setting goals, working on them and achieving them – is a major factor predicting gratifying professional success in physicians. It may also explain a common phenomenon: the outstanding physician who, at 45 or 50 years old, suddenly develops a consuming interest in trading stocks or wine making. Practicing medicine has turned into a job and no longer provides a challenge or sense of accomplishment.
Tools for Controlling Stress
A balance in mind, body and spirit is essential to the effectiveness of physician. The less energy we have, the more irritated we become, and the more our behavior can be disruptive and explosive. Proper nutrition, physical exercise, ample rest, relaxation and stress-reduction techniques provide needed balance. But self-awareness and self-management skills are just as crucial to achieving this balance.
In order to make a critical difference concerning disruptive behavior in health care organizations, preventative training and coaching programs with focus on self-management skills such as stress control, goal setting, work-life balance and personal growth should be given first priority in targeting disruptive behavior. Placing the emphasis on how to treat and manage the individuals once their disruptive behavior becomes evident may be putting the cart before the horse.
Iris Grimm, creator of the Balanced Physician Coaching and Training Program, can be reached at 770-428-2334 or at www.BalancedPhysician.com.

 Explore what our dogs can teach us about leadership:
Five Insights and Practical Applications
Explore what our dogs can teach us about leadership:
Five Insights and Practical Applications